Understanding Inner-Ear Decompression Sickness (IEDCS) for Scuba Divers
Scuba diving is a thrilling adventure that allows us to explore the mesmerizing depths of the ocean. However, it comes with its share of risks, one of which is Inner-Ear Decompression Sickness (IEDCS). In this article, we’ll delve into the world of IEDCS, demystifying medical jargon and providing crucial information for scuba divers.
The Inner Ear: A Marvel of Sensation
Before we dive into IEDCS, let’s understand the inner ear. This intricate organ, known as the vestibulocochlear organ, serves two vital functions: hearing and balance.
Imagine it as a spiral-shaped wonder surrounded by a protective bony structure. Inside, it contains a fluid called endolymph, responsible for transmitting sound and maintaining our sense of position.
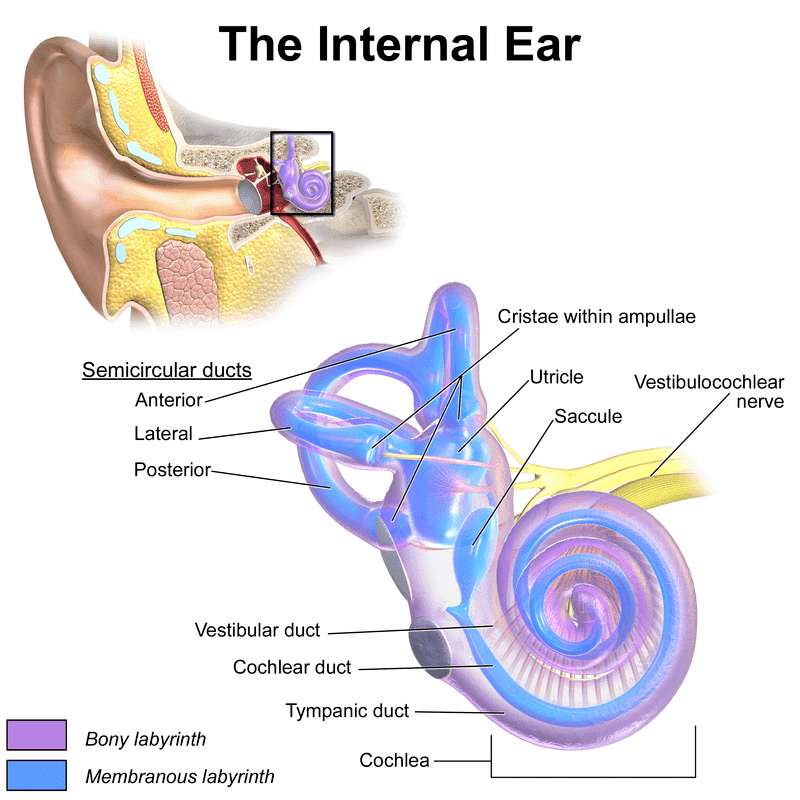
The cochlea within the inner ear translates sound waves into signals for our auditory nerve, enabling us to hear. Meanwhile, the vestibular component, consisting of the utricle, saccule, and semicircular canals, plays a pivotal role in our sense of balance and spatial orientation.
Unraveling Inner-Ear Decompression Sickness
What is IEDCS?
Inner Ear Decompression Sickness (IEDCS), also known as Vestibular DCS or Ear Bends, is a condition that occurs in compressed-gas divers. It is believed to stem from the formation of gas bubbles in the endolymphatic and perilymphatic spaces during ascents.
IEDCS Symptoms
IEDCS typically manifests within 30 minutes after surfacing and primarily affects the vestibular system.
On dives involving hypoxic trimix gasses it may manifest during the ascent; often within a short time of gas switching to an oxygen-rich decompression gas.
Divers experiencing IEDCS often report symptoms like:
- Vertigo (intense dizziness)
- Ataxia (coordination difficulties)
- Nausea and vomiting
- Impaired hearing
IEDCS Causes
While the exact cause of IEDCS isn’t fully understood, it is thought that it can result from gas bubbles precipitating in the inner ear during ascent.
Another contributing factor may be a right-to-left shunt in the heart (PFO), which can introduce gas into the labyrinthine artery, a potential culprit for the condition.
IEDCS Risk Factors and Prevalence
IEDCS is a rare occurrence among divers. It is most commonly observed in deep-diving scenarios, especially when helium-oxygen (trimix) mixtures are used.
Though its exact prevalence remains uncertain, some sources suggest an incidence of 0.2% to 0.3% per recreational dive, making it a relatively rare condition among divers.
IBCD-induced IEDCS
IEDCS can be caused due to Isobaric Counter-Diffusion (IBCD) if a technical hypoxic trimix diver switches from a helium-rich gas mixture to a rich oxygen mixture during their ascent.
- IBCD-induced IEDCS has not been observed in dives shallower than 70m.
- Gas selection techniques are taught on full trimix courses to minimize this risk.
PFO-induced IEDCS
A second cause of IEDCS, that does not involve IBCD, is related to Patent Foramen Ovale (PFO).
- PFO is a heart defect that allows blood to move between the left and right atria (upper chambers) of the heart.
- This allows inert-gas-rich blood to bypass the lungs and reduces off-gassing efficiency.
- In rare cases, the right-to-left shunt can cause an arterial gas embolism (AGE) to enter the labyrinthine artery; the primary source of blood for the inner ear.
Identifying IEDCS: Symptoms
Recognizing IEDCS is crucial for timely treatment. Symptoms typically arise within two hours of surfacing but can even occur while the diver is still underwater (IBCD).
Common symptoms include;
- Vertigo (dizziness)
- Ataxia (loss of coordination)
- Nausea
- Vomiting
- Tinnitus (ear ringing)
- Hearing loss
Identifying IEDCS: Evaluation
When evaluating a diver for IEDCS, a comprehensive neurological examination is essential. This should include assessments of;
- Balance
- Gait
- Proprioception (also known as kinaesthesia; the sense of self-movement, force, and body position)
- Nystagmus (involuntary eye movement)
- Bilateral hearing
Additionally, other diving-related injuries and decompression sickness manifestations must be considered.
IEDCS vs. Inner Ear Barotrauma
Distinguishing between IEDCS and inner ear barotrauma can be challenging.
- IEDCS involves decompression-related bubbles, whereas barotrauma involves over-pressure injury to body tissues.
- Both conditions share similar cochlear and vestibular symptoms.
- A thorough evaluation by a medical professional is necessary to differentiate between the two.
IEDCS Recovery and Prognosis
Complete recovery from IEDCS is less common compared to general decompression sickness.
- Studies have reported residual deficits in a significant percentage of patients, with vestibular deficits being more prevalent than cochlear deficits.
- Even with proper recompression therapy, some individuals may experience ongoing issues with balance and hearing.
IEDCS Conclusion
In conclusion, while scuba diving offers a world of wonder beneath the waves, it’s essential to be aware of the potential risks, including IEDCS.
- Understanding the symptoms, risk factors, and evaluation process is crucial for divers to enjoy their underwater adventures safely.
- Always prioritize safety, plan dives meticulously, and seek prompt medical attention if any symptoms arise.
References
Katharine L. Boyd; Anton A. Wray. Inner Ear Decompression Sickness. National Library of Medicine. May 1, 2023
Mitchell SJ, Doolette DJ. Pathophysiology of inner ear decompression sickness: potential role of the persistent foramen ovale. Diving Hyperb Med. 2015 Jun;45(2):105-10. [PubMed]
Mitchell SJ, Doolette DJ. Selective vulnerability of the inner ear to decompression sickness in divers with right-to-left shunt: the role of tissue gas supersaturation. J Appl Physiol (1985). 2009 Jan;106(1):298-301. [PubMed]
Klingmann C, Praetorius M, Baumann I, Plinkert PK. Barotrauma and decompression illness of the inner ear: 46 cases during treatment and follow-up. Otol Neurotol. 2007 Jun;28(4):447-54. [PubMed]
Doolette DJ, Mitchell SJ. Biophysical basis for inner ear decompression sickness. J Appl Physiol (1985). 2003 Jun;94(6):2145-50. [PubMed]
Arieli R. Taravana, vestibular decompression illness, and autochthonous distal arterial bubbles. Respir Physiol Neurobiol. 2019 Jan;259:119-121. [PubMed]
Cantais E, Louge P, Suppini A, Foster PP, Palmier B. Right-to-left shunt and risk of decompression illness with cochleovestibular and cerebral symptoms in divers: case control study in 101 consecutive dive accidents. Crit Care Med. 2003 Jan;31(1):84-8. [PubMed]
Gempp E, Louge P. Inner ear decompression sickness in scuba divers: a review of 115 cases. Eur Arch Otorhinolaryngol. 2013 May;270(6):1831-7. [PubMed]
Nachum Z, Shupak A, Spitzer O, Sharoni Z, Doweck I, Gordon CR. Inner ear decompression sickness in sport compressed-air diving. Laryngoscope. 2001 May;111(5):851-6. [PubMed]
About The Author

Andy Davis is a RAID, PADI TecRec, ANDI, BSAC, and SSI-qualified independent technical diving instructor who specializes in teaching sidemount, trimix, and advanced wreck diving courses.
Currently residing in Subic Bay, Philippines; he has amassed more than 10,000 open-circuit and CCR dives over three decades of challenging diving across the globe.
Andy has published numerous diving magazine articles and designed advanced certification courses for several dive training agencies, He regularly tests and reviews new dive gear for scuba equipment manufacturers. Andy is currently writing a series of advanced diving books and creating a range of tech diving clothing and accessories.
Prior to becoming a professional technical diving educator in 2006, Andy was a commissioned officer in the Royal Air Force and has served in Iraq, Afghanistan, Belize, and Cyprus.
In 2023, Andy was named in the “Who’s Who of Sidemount” list by GUE InDepth Magazine.
Purchase my exclusive diving ebooks!
Originally posted 2023-09-15 12:52:19.