Skin Bends: A Guide to Cutaneous Decompression Sickness
Scuba diving allows us to explore the mesmerizing underwater world, but beneath the surface, there are hidden risks that every diver should be aware of. One such risk is Decompression Sickness (DCS), a condition that can manifest in various ways, including what’s commonly known as “skin bends“.
In this article, we’ll dive deep into the issue of skin bends, also known as cutaneous DCS, to explore its symptoms, causes, risk factors, and essential information that every scuba diver should know.
Understanding Skin Bends
Cutaneous Manifestation of DCS
Skin bends, scientifically referred to as cutaneous decompression sickness, are one of the most common findings in DCS. They typically present as a distinct skin abnormality that serves as an early warning sign for divers.
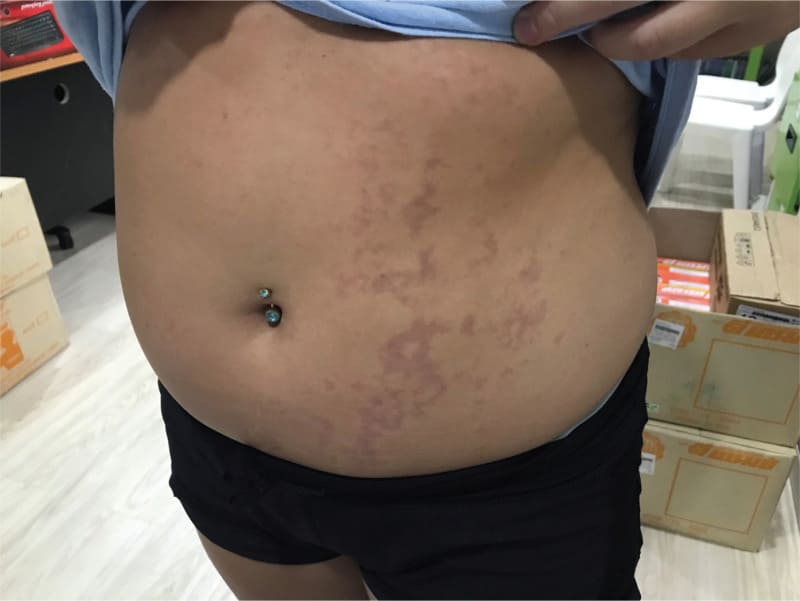
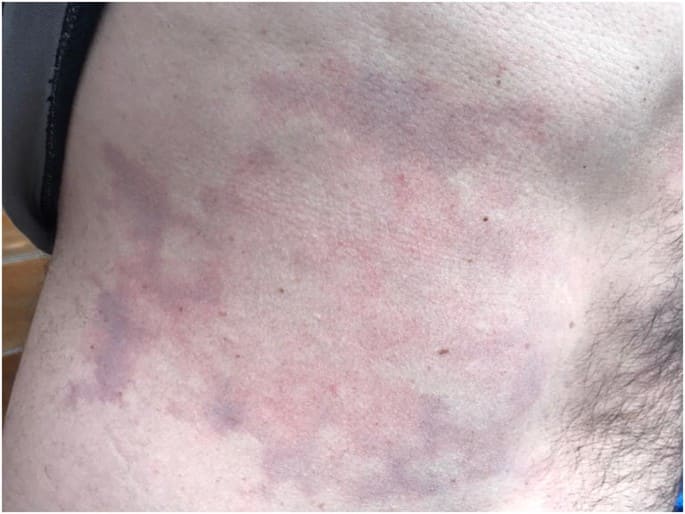
Cutis marmorata, as it’s known medically, is characterized by an erythematous (red), pruritic (itchy) rash that spreads irregularly and can deepen in color, resembling mottled, cyanotic (bluish) patches.

The underlying cause is believed to be the formation of inert gas bubbles within the body’s tissues and capillaries just below the skin.
While skin bends themselves often resolve without complications, they can indicate more severe underlying issues, such as;
- Spinal cord injury
- Pulmonary venous gas embolism
- Acute circulatory collapse
- Stroke from paradoxical arterial embolism
Skin Bends Symptoms
Recognizing the symptoms of skin bends is crucial for the safety of divers. The symptoms of cutaneous DCS may include:
- Itching, typically around the ears, face, neck, arms, and upper torso.
- A sensation of tiny insects crawling over the skin.
- Mottled or marbled skin, often appearing around the shoulders, upper chest, abdomen, and sometimes thighs, accompanied by itching.
- Swelling of the skin, often accompanied by tiny scar-like depressions known as pitting edema.
It’s important to distinguish skin bends from other skin conditions:
- While divers might describe it as similar to a rash or hives, skin bends tend to manifest as dark, mottled areas that are not raised.
- The skin can also be tender to the touch, and symptoms often include deep-tissue soreness, tenderness, bruising, or blotchiness.
Causes and Risk Factors
The exact mechanism behind skin bends remains a mystery, and predicting individual susceptibility is challenging. However, based on reports from DAN (Divers Alert Network), skin bends tend to occur in areas of the body with higher fatty tissue content, such as the;
- Abdomen
- Thighs
- Triceps area
- Buttocks
- Breasts
What’s alarming is that approximately 20 percent of divers who experience skin bends also exhibit neurological symptoms like;
- Confusion
- Visual blurring
- Memory loss.
This highlights the importance of taking cutaneous DCS seriously and seeking medical attention promptly.
Managing Skin Bends
Early Recognition is Key
Recognizing skin bends early can significantly impact your recovery. If you or a fellow diver show signs or symptoms of DCS, take immediate action:
- Suspend all diving activities.
- Initiate oxygen therapy.
- Seek medical attention.
Breathing oxygen on the surface can lead to substantial improvement, but only a qualified physician can determine whether further treatment is necessary.
Prevention Strategies
Preventing decompression sickness is always better than treating it. Here are some strategies to reduce the likelihood of skin bends and DCS:
- Use nitrox while diving air tables (ensure depth limits are observed).
- If diving with regular air, shorten bottom times by five to 10 minutes.
- Consider prolonging safety stops beyond three minutes.
- Divers experiencing repeated episodes of DCS should seek a thorough evaluation by a physician trained in dive medicine.
Skin Bends and Flying After Diving
Just like other forms of decompression sickness, divers who’ve experienced skin bends should avoid flying until cleared by a doctor familiar with diving medicine. Flying too soon after diving can worsen symptoms and pose serious health risks.
How to Recognize Skin Bends
A post-dive change in the color or texture of your skin, such as a rash or a marbled appearance, with or without an itch, may be decompression-related. Skin manifestations of DCS, also known as cutaneous DCS, are more common than you might think.
Divers often mistake cutaneous DCS for a rash due to other causes, such as contact with marine life or an allergic reaction.
However, it’s crucial to note that cutaneous DCS is often associated with neurological changes, which may sometimes be subtle. Prompt consultation with a diving medical specialist is essential to assess the situation.
Skin Bends: Onset and Evolution
Symptoms of skin bends typically occur within minutes to hours after a dive. The severity and duration of these symptoms can vary:
- Itching is usually the first symptom to resolve.
- The rash may subside within 24 hours.
- Marbling generally fades out over a few days and does not turn blue-green like a bruise.
- Lymphatic DCS may resolve on its own, but treatment can expedite the disappearance of marbling and swelling.
With prompt and appropriate oxygen first aid for around four hours, the rash and other symptoms can disappear and not recur. However, if the oxygen first aid is poor or stopped too soon, symptoms may persist or return.
Skin Bends Risk Factors
The primary risk factor for cutaneous DCS is your dive profile, particularly multiple repetitive dives with relatively short surface intervals. This pattern of diving is common amongst recreational divers on vacation or live-aboard trips.
However, divers with a patent foramen ovale (PFO) may be at increased risk. PFO is a common, congenital, generally benign hole between the heart’s left and right chambers; i.e. a left-to-right shunt.
A history of repeated cutaneous DCS often leads to the identification of an unsuspected PFO.
Skin Bends Treatment
Any skin change that might be DCS-related should be evaluated by a physician. A rash unaccompanied by other symptoms typically doesn’t need recompression treatment.
However, if your physician detects signs of neurological effects, hyperbaric oxygen treatment in a recompression chamber is usually recommended.
- Appropriate treatment for skin mottling or swelling will depend on the results of a physical examination.
- Skin changes associated with any other manifestations of DCS should be treated as an emergency.
Skin Bends Emergency Warnings
If you experience abdominal, back, or chest pain alongside skin mottling, it’s crucial to seek emergency medical attention promptly. The shorter the time between a dive and the onset of symptoms, the more likely it is that severe DCS will develop.
Remember, your safety as a diver should always be the top priority. Stay informed, recognize the signs, and take immediate action if you suspect skin bends or any other symptoms of DCS. Your well-being and enjoyment of the underwater world depend on it.
Skin Bends References
Skin Bends, by Marty McCafferty, EMT-P, DMT. Alert Diver, Q2 Spring 2012
Skin Bends and Flying After Diving. DAN, February 9, 2022
How to recognize skin bends, a recent DAN case study. DAN World, September 27, 2018
Skin Bends: a Cutaneous Manifestation of Decompression Sickness
Ronald S. Strauss, M.D. J Gen Intern Med. 2019 Oct; 34(10): 2290. Published online 2019 Jul 25. doi: 10.1007/s11606-019-05208-y
Decompression illness: clinical aspects of 5278 consecutive cases treated in a single hyperbaric unit, by Xu W, Liu W, Huang G, Zou Z, Cai Z, Xu W. PLoS One. 2012;7(11):e50079. doi: 10.1371/journal.pone.0050079. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Cutis Marmorata in Decompression Sickness by Vasileios K. N Engl J Med. 2010;362:23. doi: 10.1056/NEJMp1001616. [PubMed] [CrossRef] [Google Scholar]
About The Author

Andy Davis is a RAID, PADI TecRec, ANDI, BSAC, and SSI-qualified independent technical diving instructor who specializes in teaching sidemount, trimix, and advanced wreck diving courses.
Currently residing in Subic Bay, Philippines; he has amassed more than 10,000 open-circuit and CCR dives over three decades of challenging diving across the globe.
Andy has published numerous diving magazine articles and designed advanced certification courses for several dive training agencies, He regularly tests and reviews new dive gear for scuba equipment manufacturers. Andy is currently writing a series of advanced diving books and creating a range of tech diving clothing and accessories.
Prior to becoming a professional technical diving educator in 2006, Andy was a commissioned officer in the Royal Air Force and has served in Iraq, Afghanistan, Belize, and Cyprus.
In 2023, Andy was named in the “Who’s Who of Sidemount” list by GUE InDepth Magazine.
Purchase my exclusive diving ebooks!
Originally posted 2023-09-15 14:06:04.






On May 8, 2025 my wife = dive buddy had cutaneous symptoms of DCS. This article was very helpful. Thank you.
excellent articles…Thank You.